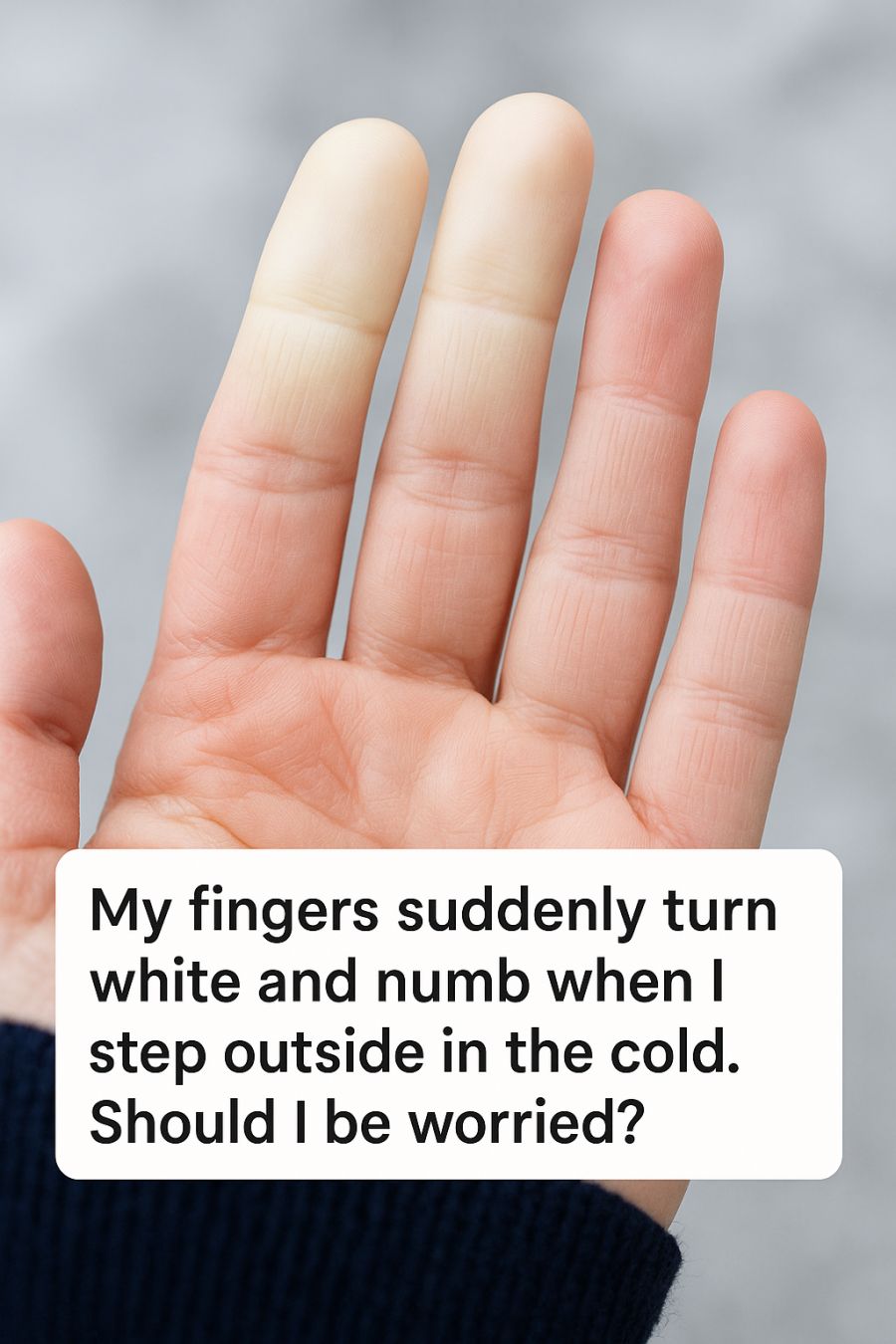
Stepping outside into the cold can be a refreshing experience for some, but for others, it can trigger an unsettling physical reaction. If you’ve ever noticed your fingers suddenly turning white and numb after being exposed to cold weather, you might have found yourself wondering whether this is a cause for concern.
While it’s easy to dismiss such symptoms as a normal response to chilly temperatures, they could potentially indicate an underlying condition. Understanding the reasons behind these sudden changes in your fingers can help you determine whether it’s something to worry about or just a harmless reaction to the cold.
A Sudden Color Change: What’s Happening to Your Fingers?
The phenomenon of fingers turning white, often followed by a numb sensation, is due to reduced blood flow. When exposed to cold, the blood vessels in your fingers constrict to preserve body heat, a process known as vasoconstriction. In some individuals, this response is exaggerated, leading to a noticeable color change.
When the blood flow is significantly reduced, the skin loses its usual pinkish hue, turning pale or white. This can be followed by a blue tint, known as cyanosis, as the oxygen levels in the blood decrease. Once warmth returns and circulation improves, the skin may turn red as blood rushes back into the area.
When Cold Fingers Are More Than Just ‘Normal’
While cold fingers are a common occurrence in chilly weather, the extent and frequency of the symptoms can signal something more serious. If your fingers frequently change color and become numb in response to cold or stress, it may indicate an underlying vascular condition.
Recurrent and severe episodes of finger color changes should not be ignored, especially if accompanied by pain or sores. It’s important to monitor the pattern and intensity of these symptoms to determine if medical intervention is necessary.
1. What Is Raynaud’s Phenomenon, Exactly?
Raynaud’s phenomenon is a condition characterized by episodic spasms of the small arteries in the extremities, most commonly the fingers and toes. These spasms reduce blood flow and cause the affected areas to change color (white, blue, and then red) and feel numb or painful.
Raynaud’s can be primary, meaning it occurs on its own, or secondary, where it is associated with other diseases such as scleroderma or lupus. Primary Raynaud’s is more common and tends to be less severe.
2. How Raynaud’s Turns Fingers White, Blue, and Red
During a Raynaud’s attack, the small arteries that supply blood to your skin begin to narrow, limiting blood circulation to affected areas. This leads to the skin turning white. As the episode progresses, a lack of oxygen causes the skin to appear blue.
Once the attack subsides and blood flow returns, the skin often turns red and may throb or tingle. This color sequence — white, blue, and red — is a hallmark of Raynaud’s phenomenon.
3. Common Triggers: Cold Weather, Stress, and Even the Fridge
Cold temperatures are the most common trigger for Raynaud’s attacks, but they are not the only ones. Emotional stress can also cause symptoms, as it leads to similar physiological responses in the body.
Surprisingly, even mild cold exposure, such as reaching into a refrigerator or holding a cold drink, can trigger an episode. It’s crucial for individuals with Raynaud’s to be aware of their triggers and take steps to avoid them.
4. Who Is Most at Risk (And Who Should Worry More)?
Raynaud’s phenomenon is more prevalent in women than men and often starts between ages 15 and 30. People living in colder climates are more likely to experience symptoms due to frequent exposure to triggering conditions.
Individuals with a family history of Raynaud’s, those with certain autoimmune or connective tissue diseases, and smokers are at a higher risk. While primary Raynaud’s is generally not a cause for significant concern, secondary Raynaud’s can be associated with more serious health issues and requires medical evaluation.
5. Warning Signs It Might Be Something More Serious
If you experience Raynaud’s symptoms accompanied by joint pain, skin rashes, or muscle weakness, it could be indicative of an underlying autoimmune condition. The presence of sores or ulcers on the fingers is also a red flag that warrants medical attention.
Persistent or worsening symptoms, especially if they lead to tissue damage, necessitate a thorough examination to rule out secondary causes and to initiate appropriate treatment.
6. Simple At-Home Hacks TikTok Loves (And Which Are Actually Safe)
Social media is full of quick fixes and hacks for managing Raynaud’s, but it’s important to approach these with caution. Simple measures like wearing warm gloves, using hand warmers, or soaking hands in warm water are safe and effective.
More unconventional methods, such as using certain food items or herbal remedies, should be approached with skepticism unless backed by scientific evidence. Always consult healthcare professionals before trying new treatments.
7. Proven Ways to Protect Your Hands in Cold Weather
To prevent Raynaud’s attacks, keeping your hands warm is key. Layering gloves and using mittens can provide extra insulation. Battery-heated gloves are also available for those who need additional warmth.
Avoiding sudden temperature changes and gradually acclimatizing to colder environments can help minimize attacks. It’s also beneficial to maintain a warm core body temperature, as this can reduce the frequency of attacks.
8. When to See a Doctor About Color-Changing Fingers
If your fingers frequently change color and become numb, or if you notice other concerning symptoms, it’s advisable to consult a healthcare provider. They can assess whether your symptoms are due to primary Raynaud’s or something more serious.
Early diagnosis and intervention are crucial for managing Raynaud’s, especially in cases where it is secondary to another condition. A healthcare provider can help tailor a treatment plan that suits your needs.
9. Tests and Diagnoses: What to Expect at the Clinic
When you visit a doctor for symptoms of Raynaud’s, they may begin with a detailed medical history and physical examination. Nailfold capillaroscopy, a test that examines the small blood vessels near your fingernails, might be performed.
Blood tests may also be ordered to check for autoimmune markers or other conditions associated with secondary Raynaud’s. These tests help distinguish between primary and secondary Raynaud’s and guide appropriate treatment.
10. Treatment Options: From Lifestyle Tweaks to Medication
Treatment for Raynaud’s often begins with lifestyle modifications, such as avoiding known triggers and keeping warm. Calcium channel blockers, a type of medication, can be prescribed to help dilate blood vessels and improve circulation.
In more severe cases, additional medications like vasodilators or surgery may be considered. Biofeedback and stress management techniques can also be beneficial, particularly for those whose symptoms are triggered by stress.
11. What Happens If You Ignore It?
Ignoring Raynaud’s symptoms, particularly if they are severe or secondary, can lead to complications. Prolonged reduced blood flow can cause tissue damage, leading to ulcers or, in rare cases, gangrene.
For those with secondary Raynaud’s, ignoring symptoms means potentially overlooking a serious underlying condition that requires treatment. Early intervention can prevent complications and improve quality of life.
12. How to Track Your Symptoms and Advocate for Yourself
Keeping a symptom diary can be invaluable in managing Raynaud’s. Note the frequency, duration, and triggers of episodes, as well as any associated symptoms. This information can help your healthcare provider make informed decisions about your care.
Educate yourself about Raynaud’s and related conditions. Being informed allows you to advocate for yourself effectively and work collaboratively with your healthcare team to manage your symptoms.