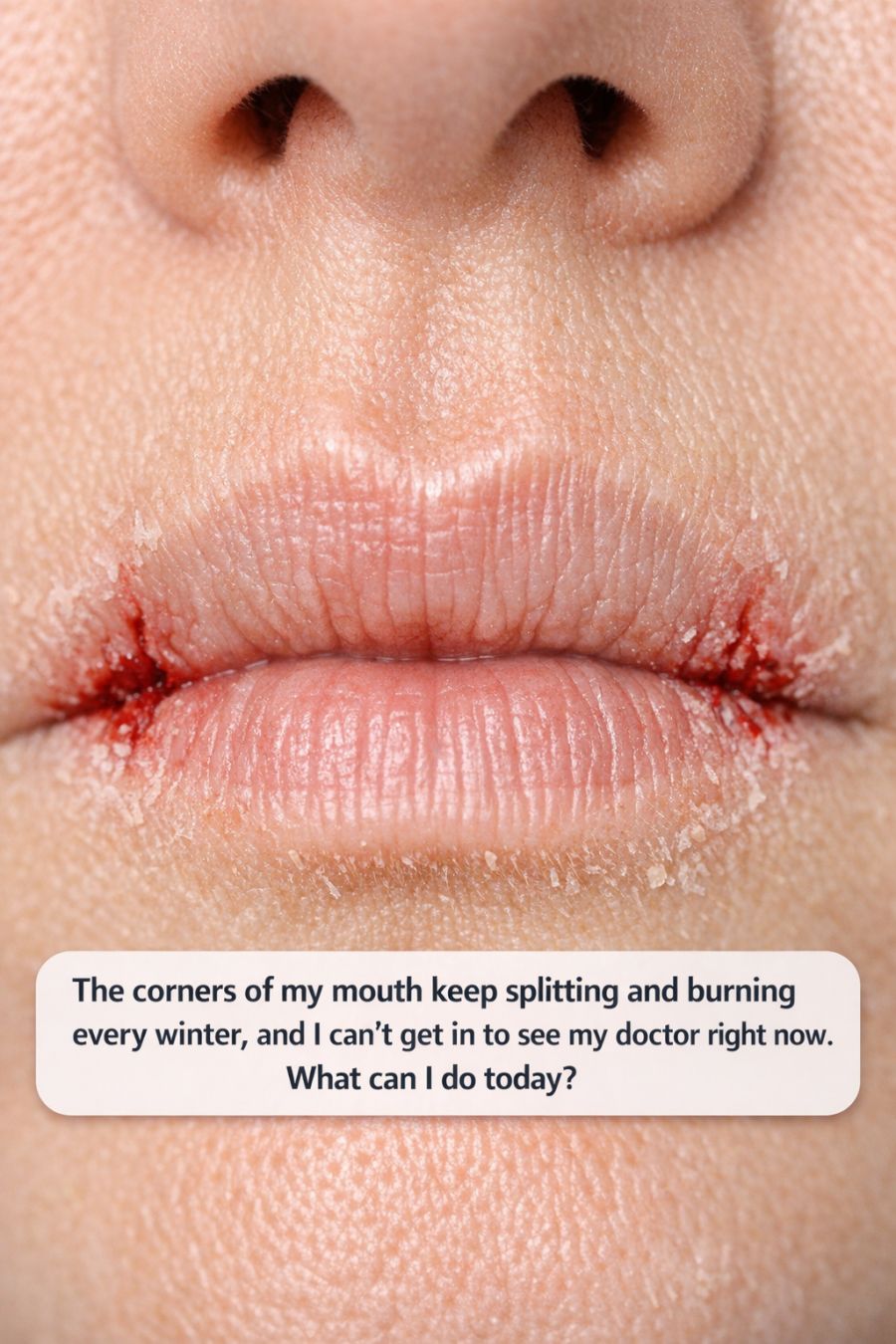
As the winter months roll in, many of us find ourselves facing a variety of skin-related issues. One common problem that affects a significant number of individuals is the splitting and burning of the corners of the mouth, medically known as angular cheilitis. This condition can be both painful and frustrating, especially when you can’t immediately get in to see your doctor. Fortunately, there are several steps you can take today to alleviate discomfort and promote healing.
In this article, we’ll explore the causes of these uncomfortable splits, how to distinguish between angular cheilitis and simple chapped lips, and effective home remedies and prevention strategies. By understanding the condition and implementing the right measures, you can manage and even prevent these painful episodes during the cold season.
1. What’s Actually Going On With The Cracks At The Corners Of Your Mouth?
Angular cheilitis is an inflammatory condition characterized by red, swollen patches in the corners of your mouth. It can be caused by a variety of factors, including fungal or bacterial infections, excessive saliva buildup, and nutritional deficiencies. The condition is often exacerbated by cold, dry weather, which leads to chapped lips and further irritation.
When saliva accumulates in the corners of the mouth, it can create a moist environment where yeast and bacteria thrive, leading to infection. Additionally, the repeated opening and closing of the mouth can cause small cracks, which become painful and slow to heal. Understanding these underlying causes is crucial to effectively treating and preventing angular cheilitis.
2. How To Tell If It’s Angular Cheilitis Or Just Chapped Lips
While both conditions result in dryness and discomfort, angular cheilitis and chapped lips have distinct characteristics. Angular cheilitis specifically affects the corners of the mouth, leading to deep cracks, redness, and sometimes crusting. Chapped lips, on the other hand, typically involve dryness and flaking of the entire lip surface.
Another distinguishing factor is the presence of pain and swelling. If you notice that the corners of your mouth are particularly tender, red, and swollen, it’s more likely to be angular cheilitis. In contrast, chapped lips generally feel dry and rough without significant swelling. Identifying these differences can help you choose the appropriate treatment.
3. The One Thing To Do First: Keep The Area Clean And Dry
Maintaining hygiene is critical when dealing with angular cheilitis. The first step is to gently clean the affected area with mild soap and water, ensuring you remove any dried saliva or crusts. Pat the area dry with a clean towel, as moisture can worsen the condition.
Refrain from licking your lips or rubbing the affected corners, as this can introduce more moisture and irritants. Keeping the area dry helps prevent the growth of yeast and bacteria, which can exacerbate the infection. Regular cleaning and drying are simple yet effective steps to kickstart the healing process.
4. Petroleum Jelly Vs. Fancy Lip Balms: What To Put On (And What To Skip)
When it comes to moisturizing and protecting the delicate skin around the mouth, petroleum jelly is often recommended for its occlusive properties. It creates a barrier that locks in moisture while keeping out irritants. Apply a thin layer to the affected area after cleaning and drying it.
Be cautious with flavored or fragranced lip balms, as these can contain ingredients that may irritate the skin further. Stick to plain, unscented options if you prefer lip balm. Avoid products with menthol or camphor, which can be drying and aggravate the condition.
5. The Overnight Trick: Healing Ointments You Can Use Right Now
For overnight relief, consider using a thick healing ointment such as Aquaphor or a hydrocortisone cream if inflammation is severe. Apply a generous amount to the corners of your mouth before bed, allowing the ointment to work while you sleep.
These ointments help to soothe irritation and reduce inflammation, promoting faster healing. Make sure to choose products that are free from potential allergens and irritants. This simple overnight routine can provide significant relief by morning.
6. Simple Kitchen Remedies: Honey, Coconut Oil, And Other Home Options
There are several natural remedies you can try at home to alleviate symptoms. Honey, known for its antimicrobial properties, can be applied to the affected area to help reduce infection risk. Leave it on for 15-20 minutes before rinsing off.
Coconut oil is another excellent option, as it provides hydration and has mild antifungal properties. Apply a small amount to the corners of your mouth several times a day. Other options include aloe vera gel and shea butter, both of which offer soothing and healing benefits.
7. Stop Licking Your Lips: Habits That Quietly Make It Worse
One of the most common habits that exacerbate angular cheilitis is licking your lips. While it may provide temporary relief, saliva quickly evaporates, leaving lips even drier than before. This creates a cycle of licking and drying that can worsen the condition.
Make a conscious effort to break this habit by keeping your lips moisturized with a suitable product, such as petroleum jelly. Additionally, avoid biting or picking at the cracked skin, as this can delay healing and introduce bacteria.
8. Check Your Products: Toothpaste, Lipsticks, And Masks That Might Be Irritating You
Certain personal care products may contain ingredients that irritate the sensitive skin around your mouth. Toothpaste with sodium lauryl sulfate or harsh whitening agents can contribute to irritation. Opt for a gentle, non-foaming toothpaste if you suspect this might be an issue.
Similarly, lipsticks and lip products with fragrances or allergens can trigger reactions. Consider switching to hypoallergenic or natural alternatives. If you wear face masks regularly, ensure they are clean and made from breathable materials to prevent irritation.
9. Boosting From The Inside: Iron, B Vitamins, And Hydration
Nutritional deficiencies, particularly in iron and B vitamins like B2 (riboflavin) and B12, can contribute to angular cheilitis. Consider incorporating foods rich in these nutrients into your diet, such as leafy greens, eggs, and lean meats.
Staying hydrated is also essential for maintaining healthy skin. Aim to drink at least 8 cups (64 ounces) of water per day to keep your skin and lips well-hydrated. If you suspect a deficiency, consult a healthcare professional about supplementation.
10. When You Might Need An Antifungal Or Mild Steroid Cream
In some cases, over-the-counter treatments may not be sufficient, and an antifungal cream might be necessary if a yeast infection is present. Products containing clotrimazole or miconazole can be effective against fungal infections.
If inflammation is severe, a mild steroid cream such as hydrocortisone may be recommended to reduce swelling and irritation. However, use these treatments only under the guidance of a healthcare professional to avoid potential side effects.
11. Smart Winter Prevention: Small Daily Tweaks To Stop The Cracks Coming Back
To prevent angular cheilitis from recurring, make small daily adjustments to your routine. Use a humidifier in your home to combat dry indoor air, and apply a protective lip balm or petroleum jelly before heading outdoors.
Wear a scarf or mask to shield your face from harsh winds and cold temperatures. Additionally, establish a skincare routine that includes gentle cleansing and moisturizing. These proactive measures can help keep your lips and mouth corners healthy throughout the winter months.
12. Red Flags: When Splitting Corners Mean You Should Push For Medical Help
While most cases of angular cheilitis can be managed at home, certain symptoms warrant professional medical attention. If you experience severe pain, extensive swelling, or signs of infection such as pus, it’s time to seek help.
Additionally, if the condition persists despite self-care measures or is accompanied by other symptoms like fever or weight loss, consult a healthcare provider. Persistent angular cheilitis may be a sign of an underlying health issue that requires further investigation.