Discovering a new mole on your body can be an unsettling experience, particularly if it appears to have irregular features such as uneven edges or a dark coloration. While moles are common skin growths, certain changes in their appearance can raise concerns about skin cancer, including melanoma, a potentially serious form of the disease. Unfortunately, with the holiday season approaching, getting a prompt appointment with a dermatologist might be challenging, leaving you in a state of uncertainty.
Understanding the nature of moles and what changes to watch for can empower you to make informed decisions about your health. While waiting for a professional evaluation, there are practical steps you can take to assess the mole yourself and monitor any changes. This article will guide you through what to look for, how to manage your concerns, and when to seek urgent medical attention.
1. Why A New Dark, Uneven Mole Deserves Your Attention
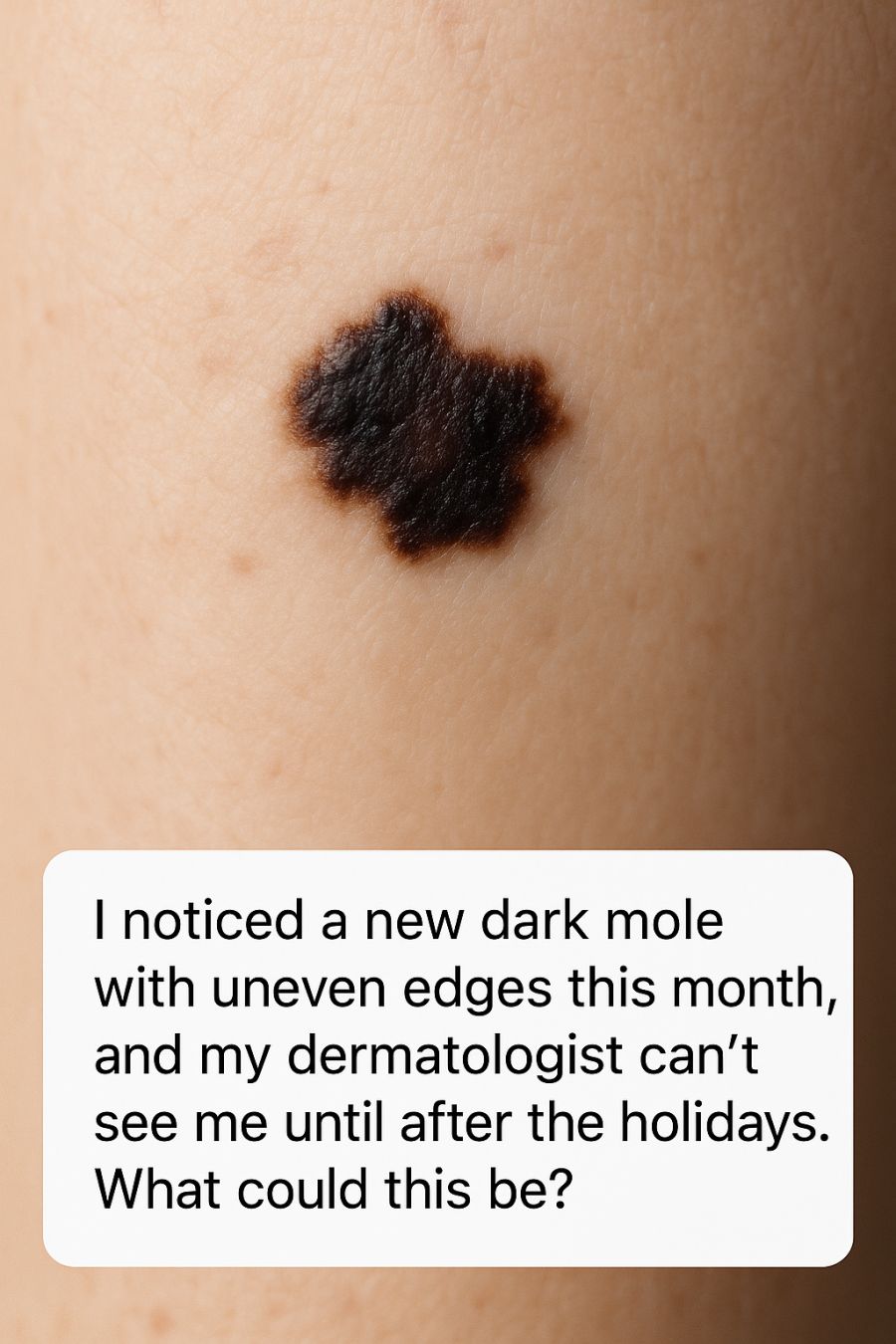
Moles, or nevi, are usually benign skin growths that develop from melanocytes, the pigment-producing cells in the skin. While most moles are harmless, a new mole or changes in an existing mole can sometimes indicate skin cancer. Dark moles with uneven edges can be of particular concern, as these are characteristics associated with atypical moles or melanoma.
Melanoma is less common than other types of skin cancer but is more likely to spread if not caught early. The irregularity of the edges and a darker color might suggest that the mole is atypical. It is important to be vigilant, especially if the mole is larger than 6 millimeters in diameter, roughly the size of a pencil eraser.
2. Understanding Atypical Moles (Dysplastic Nevi)
Atypical moles, also known as dysplastic nevi, differ from common moles in several ways. They may be larger than normal moles, have indistinct or irregular borders, and display a mix of colors ranging from tan to dark brown. These moles can appear anywhere on the body, though they are commonly found on the trunk.
Having multiple dysplastic nevi can increase your risk of developing melanoma, particularly if there is a family history of the condition. Monitoring atypical moles for any changes in size, shape, color, or texture is crucial in detecting melanoma at an early stage.
3. The ABCDE Rule: Quick At-Home Check for Suspicious Moles
The ABCDE rule is a helpful tool for assessing moles for signs of melanoma. ‘A’ stands for asymmetry, where one half of the mole does not match the other. ‘B’ is for border irregularity; watch out for edges that are ragged or blurred. ‘C’ refers to color, with concern for moles that have multiple shades or hues.
‘D’ stands for diameter, highlighting moles larger than 6 millimeters as potentially concerning. Lastly, ‘E’ is for evolving, indicating any changes in the mole over time, including size, shape, or symptoms such as itching or bleeding. If a mole exhibits any of these characteristics, further evaluation by a dermatologist is recommended.
4. What Melanoma Can Look Like in Real Life, Not Just Textbook Photos
Melanoma can present in various ways, often deviating from the textbook appearance of a uniformly dark and irregular mole. In real life, melanomas can be flat or raised, and may exhibit shades of pink, red, or even blue-black. They can also appear as a new spot on the skin that grows quickly or changes rapidly over weeks to months.
Some melanomas can mimic the appearance of benign moles, making it crucial to pay attention to any new or changing skin lesions. The key is to be aware of your skin and note any changes, as early detection significantly improves treatment outcomes.
5. Benign Possibilities: When a New Mole Is Likely Harmless
Not all new or changing moles are cause for alarm. Some benign possibilities include seborrheic keratoses, which are non-cancerous growths that can appear wart-like and vary in color from light tan to black. Cherry angiomas, small red to purple growths, are also benign and common, especially with age.
Common moles can appear during childhood and adolescence, and it’s normal for them to change slightly over time. However, if a mole’s appearance is consistent with other benign moles and it passes the ABCDE rule, it may not require immediate concern.
6. Red-Flag Changes You Should Monitor Day by Day
Keep a close eye on the mole for any changes in size, shape, or color. Look for symptoms such as itching, tenderness, or bleeding. A mole that begins to crust or scab, or develops a notch or ulceration, should be evaluated as soon as possible.
Documenting these changes with photographs and notes can be helpful for both your own monitoring and for discussing the changes with your dermatologist when you are able to see them.
7. How Urgent Is This? When to Push for a Sooner Appointment
Certain changes in a mole may warrant a more urgent visit to your dermatologist. Rapid changes in a mole’s appearance, such as growth over a few weeks or the development of symptoms like bleeding or persistent itching, should be communicated to your healthcare provider. They may be able to prioritize your appointment based on these concerns.
If you have a personal or family history of melanoma, or if you have multiple atypical moles, it’s important to convey this information to your dermatologist, as it may influence the urgency of your appointment.
8. Smart Smartphone Hacks: Photographing and Tracking Your Mole
Using your smartphone to document the mole can be an effective way to monitor changes over time. Take clear, close-up photos of the mole from different angles, ensuring good lighting and focus. It may be helpful to include a ruler or coin in the photo for scale.
Regularly photographing the mole, such as weekly or biweekly, can help track its evolution. Use a note-taking app to record any symptoms or changes you observe, which can be invaluable information for your dermatologist.
9. What Not to Do: Viral Home Remedies and TikTok “Mole Removal” Tricks to Avoid
Avoid attempting to remove or treat the mole with home remedies or DIY methods seen online, as they can cause harm and potentially delay proper diagnosis and treatment. Viral trends like using apple cider vinegar or cutting the mole off are not safe and could lead to infection or scarring.
It’s essential to rely on professional medical advice rather than unverified online sources. Trust a qualified dermatologist to evaluate and, if necessary, remove or biopsy the mole safely.
10. Teledermatology and Online Second Opinions While You Wait
Teledermatology can be a valuable resource if you cannot see your dermatologist in person promptly. Many healthcare providers offer virtual consultations where you can share images of the mole and discuss your concerns.
Online platforms also exist where you can seek second opinions from board-certified dermatologists. These services can provide additional insights and guidance while you wait for an in-person evaluation.
11. How Your Dermatologist Will Evaluate and Possibly Biopsy the Mole
During your appointment, your dermatologist will perform a thorough skin examination and assess the mole using tools like a dermatoscope, which magnifies the lesion and allows for better visualization of its features. They will evaluate the mole based on its appearance and any changes you’ve documented.
If the mole appears suspicious, your dermatologist may recommend a biopsy, where a small sample of the mole is removed and analyzed in a lab for signs of cancer. This procedure is typically quick and done under local anesthesia.
12. Lowering Your Skin Cancer Risk While You Wait to Be Seen
While waiting for your appointment, take steps to protect your skin from further damage. Use broad-spectrum sunscreen with an SPF of 30 or higher, wear protective clothing, and seek shade when outdoors. Avoid tanning beds, as they increase the risk of skin cancer.
Regularly examine your skin for new or changing moles, and encourage family members to do the same. Early detection is key in managing skin cancer risk effectively.
13. When to Go Straight to Urgent Care or the ER
If the mole begins to bleed profusely, becomes significantly painful, or shows signs of infection such as pus or spreading redness, it may require immediate medical attention. In such cases, visiting urgent care or the emergency room can ensure timely evaluation and management.
While most moles do not require emergency care, any sudden or severe changes warrant prompt attention to rule out serious conditions and to provide peace of mind.