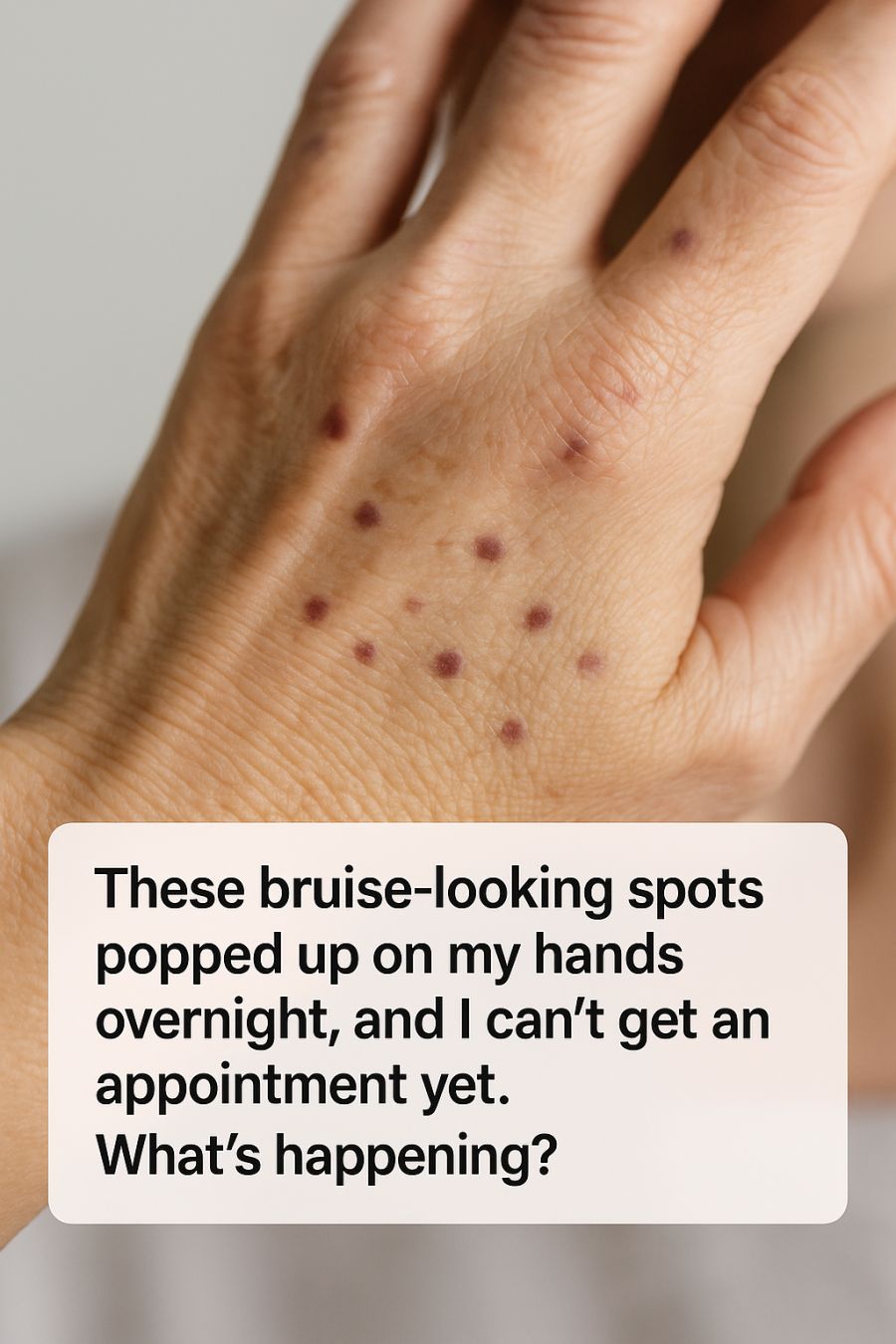
Waking up to discover bruise-like spots on your hands can be an unsettling experience, especially when they appear overnight without any apparent cause. These spots can range in color from a light purple to a deep red, and while they might resemble bruises, they often lack the telltale tenderness we associate with injuries. For many, the first instinct is to book a doctor’s appointment, but what if that isn’t an immediate option?
In this article, we’ll explore the potential causes of these mysterious marks, focusing particularly on actinic purpura, a common skin condition that affects many as they age. We’ll also delve into what you can do while waiting for a professional evaluation, including at-home care strategies and when to seek more urgent medical attention.
1. Why Sudden Bruise-Like Spots on Your Hands Are So Common as You Age
As we age, our skin undergoes numerous changes due to intrinsic factors, like the natural aging process, and extrinsic factors, such as sun exposure. One of the most common skin changes seen in older adults is the development of bruise-like spots, especially on areas frequently exposed to sunlight, such as the hands and forearms. This phenomenon is primarily due to a combination of thinning skin and weakened blood vessels.
Thinning skin, which loses about 20% of its thickness between the ages of 30 and 80, becomes less effective at cushioning the impact of minor bumps or injuries. Additionally, the collagen and elastin fibers that provide structural support to the skin gradually degrade, making the skin more fragile and susceptible to damage.
2. What Actinic Purpura Is and Why Doctors Call It ‘Senile Bruising’
Actinic purpura, often referred to as ‘senile purpura’, is a condition commonly associated with aging. It manifests as dark purple or red spots on the skin, typically on the hands, forearms, and sometimes the face. This condition is caused by the rupture of small blood vessels under the skin, a process that becomes more frequent as the structural integrity of these vessels declines with age.
Doctors often use the term ‘senile bruising’ to describe actinic purpura because it predominantly affects the elderly. The spots can appear suddenly and may take several weeks to fade, though they do not usually cause pain. While they may be cosmetically concerning, they are generally harmless and do not indicate any underlying health issues.
3. How Years of Sun Exposure Quietly Damage the Blood Vessels in Your Skin
The role of sun exposure in skin aging is significant. Ultraviolet (UV) radiation from the sun accelerates the breakdown of collagen and elastin fibers in the skin, which are crucial for maintaining its strength and elasticity. Over time, chronic sun exposure leads to a condition known as solar elastosis, where the skin becomes thickened and wrinkled.
This degradation also affects the small blood vessels in the skin’s dermal layer. As these vessels become more fragile, they are more prone to breaking even with minimal trauma. This explains why actinic purpura is most commonly found on sun-exposed areas, where UV damage is most pronounced.
4. Why These Spots Look Like Bruises but Don’t Behave Like Typical Injuries
Despite their appearance, actinic purpura spots differ from typical bruises in several ways. Traditional bruises are the result of blood vessel damage due to a significant impact, leading to pain, swelling, and color changes as the body heals. In contrast, the spots from actinic purpura generally do not cause pain or swelling.
These spots also tend to develop without a noticeable trigger, such as a fall or a bump, which can be alarming. Their persistence, often lasting for weeks, and lack of associated symptoms like tenderness, help differentiate them from common bruises.
5. Common Triggers: From Bumping a Countertop to Simply Pulling Off a Sweater
For those with actinic purpura, even the most minor physical stimuli can result in the appearance of these bruise-like spots. Everyday activities, like bumping into a countertop or pulling off a snug sweater, can cause enough stress on the fragile skin to result in vessel rupture.
Because the skin and vessels are already compromised, these seemingly innocuous actions can lead to a cascade of small, painless hemorrhages under the skin, manifesting as multiple purpura spots. Awareness of these triggers can help individuals take preventive measures, such as wearing protective clothing or padding vulnerable areas.
6. Medications and Supplements That Can Make Actinic Purpura Much Worse
Certain medications and supplements can exacerbate the symptoms of actinic purpura. Blood thinners, such as aspirin or warfarin, can increase the likelihood of bleeding under the skin, making the spots more frequent and prominent. Similarly, non-steroidal anti-inflammatory drugs (NSAIDs) can have a similar effect.
Additionally, supplements such as fish oil and vitamin E, known for their blood-thinning properties, may also contribute to increased bruising in susceptible individuals. It’s crucial for individuals to inform their healthcare providers about all medications and supplements they are taking, as adjustments might be necessary to manage actinic purpura effectively.
7. Warning Signs It Might Not Be Actinic Purpura and You Should Seek Urgent Care
While actinic purpura is generally harmless, there are instances where similar symptoms could indicate a more serious condition. If the spots are accompanied by additional symptoms such as spontaneous bleeding from other areas, significant swelling, or if they appear suddenly in large numbers, it is advisable to seek medical attention promptly.
Other warning signs include the development of systemic symptoms such as fever, fatigue, or unexplained weight loss, which may suggest an underlying hematological disorder or other serious conditions. In such cases, a comprehensive medical evaluation is necessary to rule out other potential causes.
8. What Dermatologists Do (and Don’t) Test for When You Finally Get an Appointment
During a dermatology appointment, the specialist will typically start with a thorough examination of the skin to assess the spots and any other related symptoms. The dermatologist may inquire about your medical history, including sun exposure habits, medication use, and any family history of similar conditions.
In most cases, a visual assessment is sufficient to diagnose actinic purpura, and further testing may not be necessary. However, if the dermatologist suspects another condition, they might order blood tests to check for clotting disorders or other systemic issues. Skin biopsies are rarely needed unless there is suspicion of another underlying skin condition.
9. Viral Bruise ‘Cures’ on Social Media: What Helps, What’s Harmless, and What to Avoid
Social media is rife with home remedies and ‘cures’ for various ailments, and bruising is no exception. While some suggestions, such as applying a cool compress or using arnica gel, may help reduce the appearance of bruises, they are unlikely to have a significant impact on actinic purpura.
It’s important to approach these viral cures with caution, especially those that suggest using harsh or unproven substances. Avoid remedies that involve skin irritation or those that promise quick fixes, as they may cause more harm than good. Consulting with a healthcare professional before trying new treatments is always the best course of action.
10. At-Home Care: Protecting Fragile Skin Until You Can See a Doctor
While waiting for a professional evaluation, there are several steps you can take to protect your skin and manage symptoms at home. Keeping the skin moisturized with a gentle, fragrance-free lotion can help maintain skin barrier function and reduce the risk of further damage.
Wearing long sleeves and protective clothing can shield the skin from minor trauma and additional sun exposure. For those on blood-thinning medications, it may be beneficial to discuss potential dosage adjustments with a healthcare provider to balance the risk of bleeding with the need for the medication.
11. Long-Term Strategies to Prevent New Spots and Protect Sun-Damaged Skin
Preventing further damage and the appearance of new spots involves adopting sun protection habits and skin care practices. Regular use of broad-spectrum sunscreen with an SPF of at least 30 can protect against further UV damage. Wearing protective clothing and seeking shade during peak sunlight hours are also effective strategies.
Maintaining a healthy lifestyle with a balanced diet rich in antioxidants can support overall skin health. Additionally, avoiding smoking and excessive alcohol consumption can further reduce the risk of skin damage and contribute to healthier skin aging.
12. When Bruise-Like Spots Signal a Bigger Health Issue Beyond Your Skin
In some cases, bruise-like spots may be indicative of underlying health issues that extend beyond dermatological concerns. Conditions such as blood clotting disorders, liver disease, or certain types of cancer can present with similar symptoms. These systemic conditions often come with additional signs, such as unexplained bruising on other parts of the body, persistent fatigue, or changes in skin texture.
If there is any suspicion that the spots may be related to a more serious health issue, it is crucial to seek medical evaluation promptly. Comprehensive blood work and a thorough physical examination can help determine the root cause and guide appropriate treatment.